Designing care for the underserved
How can we design a Hepatitis C wellness program that meets people where they are?
San Francisco City Hall lit up on World Hepatitis Day / Image courtesy of SF Hepatitis C Task Force
Project Title: Hepatitis C Wellness Program Design
Company: San Francisco AIDS Foundation Duration: June 2016 - Dec 2016 (6 months)
Key Project Activities: My Role: Researcher & Program Designer
User research (quantitaive and qualitative) Collaborators: SFAF staff and clients, SF Dept. of Public Health
Patient journey mapping
Brainstorming & ideation session
Program design & execution
Public advocacy
Context & Challenge
San Francisco is home to one of the most diverse and inclusive populations in the United States. The city is known for its progressive policies and was at the forefront of the movement to create needle exchange programs for People Who Inject Drugs (PWID). These programs steer away from a punitive approach and are based on the principle of harm reduction - “a public health philosophy that seeks to reduce the harms associated with both drug use and ineffective, racialized drug policies” (Drug Policy Alliance). In other words, these programs acknowledge the dignity and autonomy of people who use drugs, understand that promoting abstinence is not always a rational or viable option, and develop programs that seek to minimize harms associated with drug use. The San Francisco AIDS Foundation (SFAF) has provided street-based syringe access services to people who inject since 1993 and is one of the nation’s largest harm reduction programs.
I was hired by the Syringe Acess Services (SAS) team to assist in developing a new Hepatitis C wellness program. PWID continue to be stigmatized and face barriers to quality care, and many of them live with Hep C but are either unaware of it or resistant to getting tested. Our goals for the program design were to motivate PWID to get tested for Hep C, participate in receiving free Hep C treatment through the SFAF program, and avoid reinfection through safer injection practices.
Image courtesy of SFAF
Image courtesy of SFAF
PROCESS
Research
Traditional Hep C treatment programs may have certain assumptions about patients that are not applicable for PWID in San Francisco or may complicate their care journey. Many of these PWID are homeless or live in transitional housing, have other comorbidities such as HIV, suffer from behavioral health issues, use other substances, or may engage in other high-risk behaviors. Hep C treatment involves taking a pill everyday until Sustained Viral Response (undetectable Hep C) 12 weeks after treatment (SVR-12) is achieved, and for example, housing instability may make medication storage difficult. The first step in designing a wellness program for this group was conducting deep user research. Along with the Hep C and SAS teams, I assisted in conducting this rigorous research by going to where our patients already were - at needle exchange sites, soup kitchens, and in homeless street camps in the San Francisco Tenderloin neighborhood. Data was collected through the following methods:
Quantitative research: Needs assessment surveys
Qualitative field research: Informal interviews and in-context observations
Image courtesy of SFAF
Image courtesy of Martin de Porres House of Hospitality
Program Development
The next phase was research synthesis and sensemaking to develop insights for program development. We conducted the following activities to develop the program:
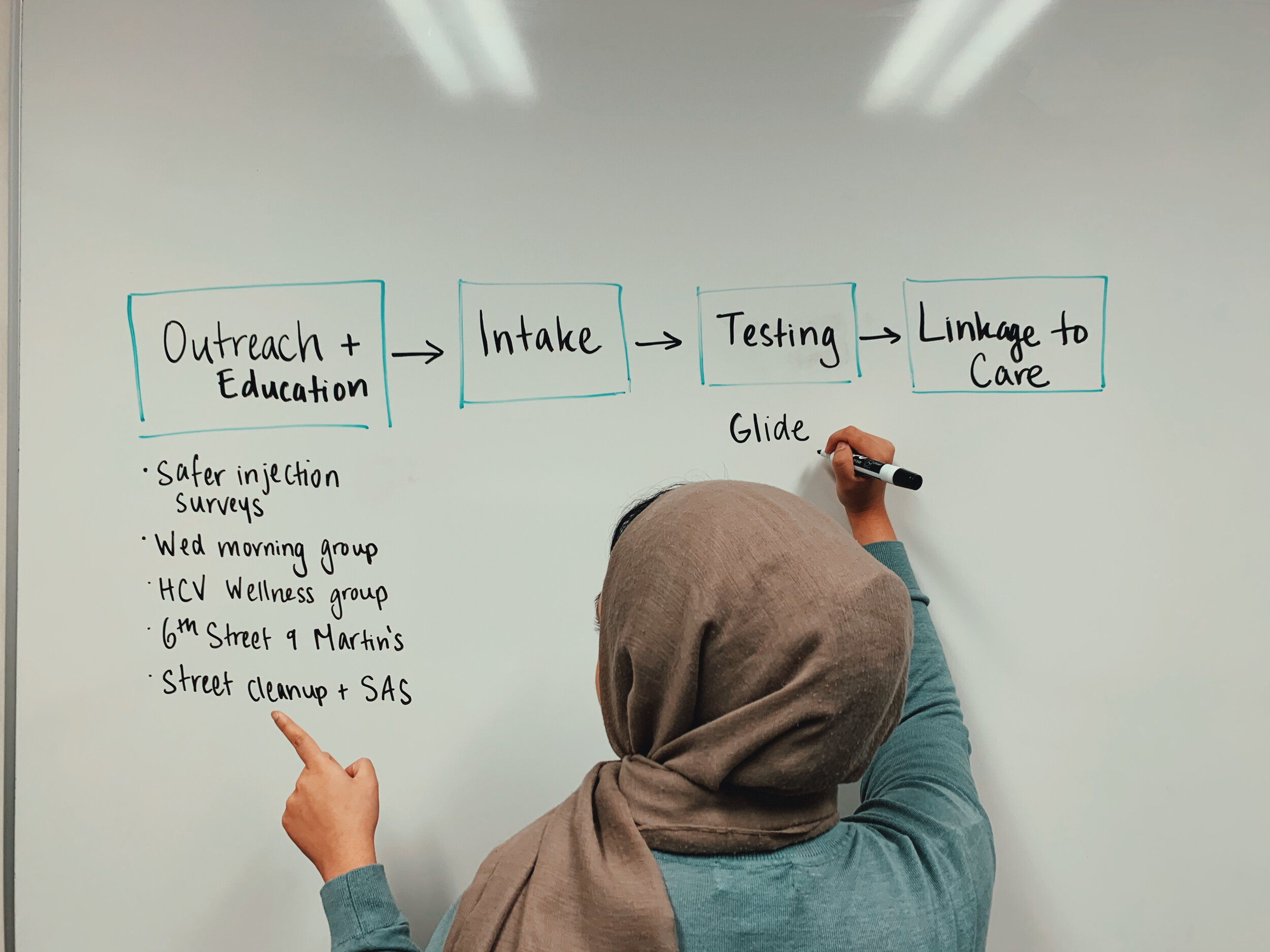
Hep C Patient Journey Mapping: to understand the unique journey for this user group and identify barriers and facilitators to care
Program Design:
Outreach, education, and recruitment efforts through needle exchange sites, wellness groups, and street syringe cleanup teams
Systemized patient intake through a Treatment Readiness Checklist we developed
Hep C testing through local partners that provided these services
Linkage to Hep C care through partnerships with neighborhood clinics and pharmaceutical companies that provided free medication
Documentation and Case Management:
I created a patient workflow and documentation system that was approved by the San Francisco Department of Public Health (SFDPH) to track patients as they went through our treatment program
I assisted in managing the patient case load by accompanying patients to their appointments, participating in wellness groups, and following up with them on their treatment
The small scale of our program allowed us to provide quality, individualized care for each client. We built trust in the community and attracted more clients to our program, empowering them and providing support through frequent follow-up meetings and bi-weekly groups that provided motivational support and safe injection tips.
Image courtesy of SFAF
Public Advocacy
In addition to our program development, the Hep C team at SFAF engaged in public advoacy efforts for Hepatitis C awareness in partnership with the San Francisco Deparment of Public Health (SFDPH), the SF Hepatitis C Task Force, and End Hep C SF. This involved public flyering, chalking sidewalks, and attending public demonstrations. The photos below are from a public demonstration on World Hepatitis Day 2016 held at the San Francisco City Hall.
Outcomes & Impact
We were successful in developing a Hep C Wellness program that was contextually relevant for our patient population, and more importantly, people were getting cured! We were able to successfully assist clients through the program, from the initial intake to Sustained Viral Response (undetectable Hep C) 12 weeks after treatment through trust-building and vigilant follow-up. The program grew to over 40 participants in the 6 months I worked with SFAF. In collaboration with the End Hep C SF initiative, we were able to raise awareness about Hepatitis C at the San Francisco city level and sustain funding to our program.
Click here to see how the program had developed over the last few years!